Up to 280 patients from seven countries will be recruited globally for the trial
Jane Kirby | Originally Published on The United Kingdom’s “Independent” Newspaper 2025
Saturday 06 December 2025 00:01 GMT
A groundbreaking trial for a prostate cancer treatment with fewer side effects has launched in the UK.
Backed by the Government-funded National Institute for Health and Care Research (NIHR), the trial will examine whether Aquablation – a therapy using robotics, AI and real-time imaging – works as well or better than traditional surgery, known as radical prostatectomy.
Radical prostatectomy involves removing the entire prostate gland in a bid to cure men of prostate cancer. The treatment is suitable for men whose cancer has not spread outside of the prostate gland or has spread to the area just outside the gland.
However, the operation carries a risk of serious side-effects, such as infection, erectile dysfunction and urinary problems.
Researchers hope Aquablation will minimise these issues.
The therapy is currently used in some centres to treat benign prostatic hyperplasia (BPH).
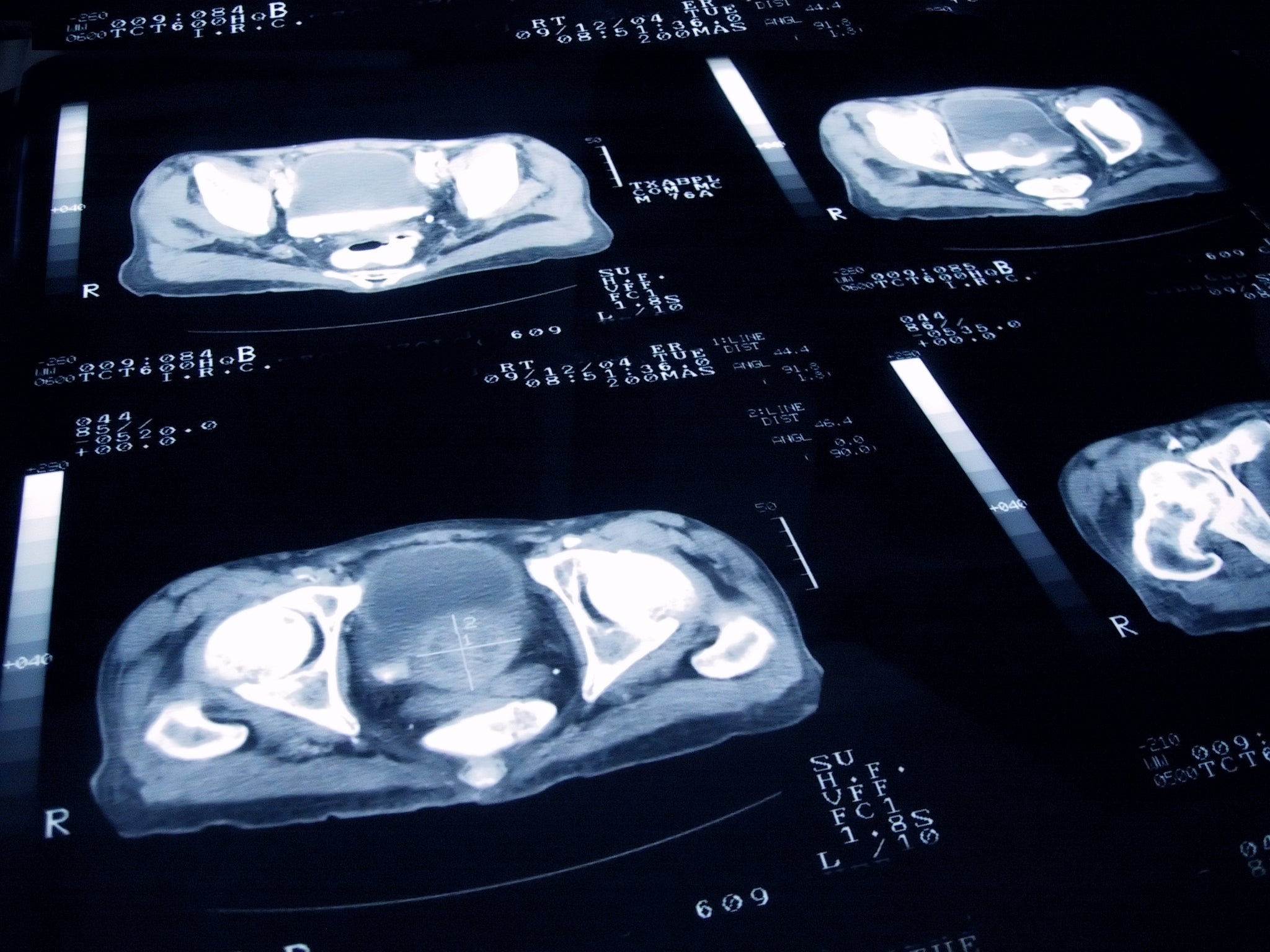
Aquablation involves a robotic-assisted, high-pressure waterjet. Surgeons can also map the entire prostate in real time with ultrasound.
Using the technique, medics find cancerous tissue to remove while avoiding surrounding nerves and muscles associated with erectile function and the bladder.
The Royal Marsden NHS Foundation Trust in London is the first hospital in Europe to recruit a patient to the trial, which is being run in seven countries.
Overall, 280 patients will be recruited globally, all with early-stage, localised prostate cancer who have already decided to have surgery.
Philip Charlesworth, consultant urological surgeon at the Royal Marsden, said: “For men with prostate cancer confined to the prostate, curative options are excellent, however, we are becoming increasingly focused on the side-effects of the cancer treatment and how we can embrace new technology to maintain a man’s quality-of-life following their surgery.
“This trial is measuring Aquablation therapy, which uses a robotic approach to surgically remove the cancer, and to preserve a man’s ability to remain continent and maintain sexual activity.
“The potential for this trial is very exciting. It has an opportunity, depending on the results of the study, to add an alternative surgical treatment option for patients with localised prostate cancer across the globe.
“The ultimate aim, and my passion, is to improve prostate cancer treatments so that they cause less harm and are less invasive for the patient.
“I feel that this is an incredibly exciting prospect for the future of prostate cancer care.”

Other potential treatments for localised prostate cancer include active surveillance or monitoring of the cancer and radiation.
The new trial is sponsored by the US company, Procept BioRobotics.
To date, there are more than 25 centres globally recruiting patients for the trial.
The four UK centres are the Royal Marsden, Guy’s and St Thomas’ NHS Foundation Trust, the Royal Free London NHS Foundation Trust and Norfolk and Norwich University Hospitals NHS Foundation Trust.
The trial comes after Health Secretary Wes Streeting said earlier this week he was “surprised” by the decision from scientific advisers to limit prostate cancer screening.
In a draft recommendation, the UK National Screening Committee (UKNSC), which advises the Government, said prostate cancer screening should not be made routinely available for the vast majority of men in the UK.
It said it would not recommend population screening using the prostate-specific antigen (PSA) test because it “is likely to cause more harm than good”.
Experts are expecting data within two years from a large trial launched by Prostate Cancer UK into whether combining PSA with other tests, such as rapid MRI scans, could lead to a recommendation for population-wide screening.
For now, the committee will put forward only a recommendation to screen men with BRCA1 and BRCA2 genetic mutations – which puts them at far higher risk of prostate cancer – every two years, between the ages of 45 and 61.
Main symptoms of prostate cancer
Prostate cancer usually starts to grow on the outer part of the prostate. If this happens, it can cause changes to the way you pee, such as:
- finding it difficult to start peeing or straining to pee
- having a weak flow of urine
- “stop start” peeing
- needing to pee urgently or often, or both
- feeling like you still need to pee when you’ve just finished
- peeing during the night
Other symptoms can include:
- erectile dysfunction (being unable to get or keep an erection)
- blood in your urine or blood in your semen
- lower back pain and losing weight without trying to (these may be symptoms of advanced prostate cancer)
Speaking on Wednesday on BBC Breakfast, Mr Streeting said he was surprised by the decision.
He said: “I’m looking very carefully at why the national screening committee reached that decision.
“I’ve always said these things have got to be based on science and evidence, not on politics.
“But the recommendation did surprise me.
“This is contested. I’ve got people in the prostate cancer community and not just really prominent patients and celebrities and politicians who’ve used their experience and their voice in this debate, but among scientists and researchers.
“This is a draft recommendation. They consult on this for three months, and then we have to make a final decision.
“What I’m going to do is get some of those leading, best scientific voices and competing opinions around the table to thrash this out, to really interrogate the data and make sure that when I come on your programme having made a decision, it’s the right decision for the right reasons, the best evidence and the public can then understand why we’ve made the decision and the scientific community can understand why we’ve made the decision.
“But I am interrogating this data and recommendation because it did surprise me.”
Many experts argue that the PSA test is not very reliable because men with a high PSA level may not have cancer, and some men with cancer have a normal PSA result.
A positive test result may lead to unnecessary treatment for slow-growing or harmless tumours, leaving men at risk of side effects such as incontinence and erectile dysfunction.
But others argue that current evidence supports wider testing.



